- 1 (888) 843-5832
- info@dnaconnexions.com
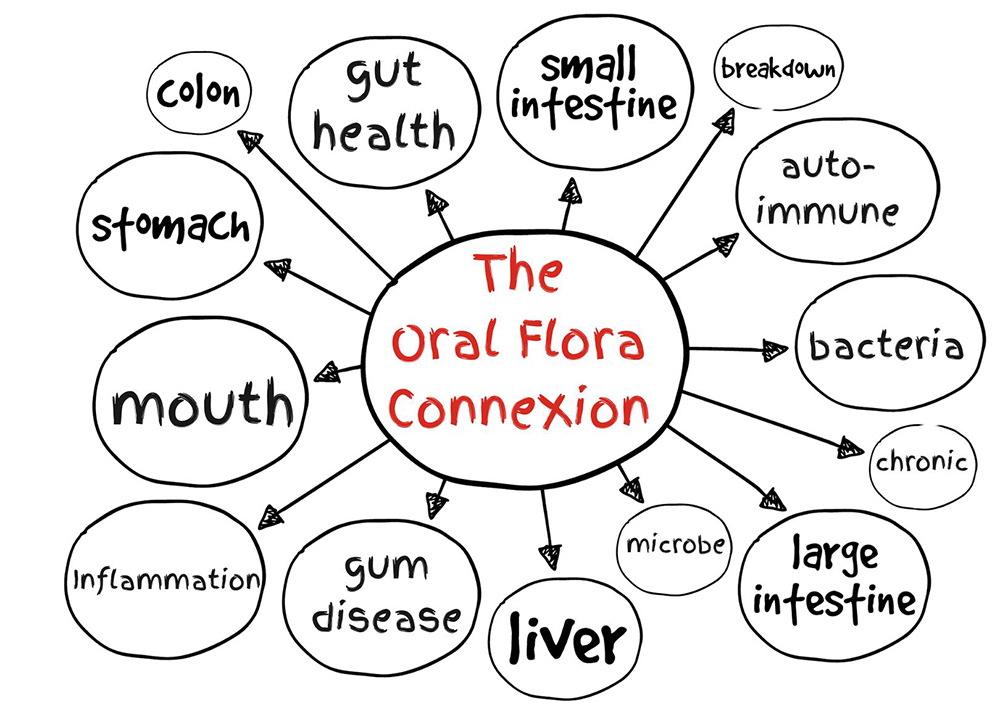
When it comes to maintaining your overall health, most people think of diet, exercise, and sleep. But there’s another critical factor that is often overlooked: oral health. Surprisingly, the bacteria in your mouth play a significant role in your gut health—and by extension, your overall well-being. In this post, we’ll explore the fascinating link between mouth bacteria and gut health, and what you can do to support both.
The Microbial Highway: From Mouth to Gut
Your mouth hosts a diverse community of over 700 bacterial species—many of which play a vital role in keeping you healthy. But the oral cavity isn’t just about teeth and gums; it serves as the entry point to your entire digestive system. Every time you swallow, you transport countless microbes from your mouth down to your gut. This constant flow means your oral microbiome—the complex ecosystem of bacteria in your mouth—has a direct influence on the microbial balance and overall health of your gastrointestinal tract.
How Oral Bacteria Affect the Gut
1. Imbalance and Inflammation
If harmful bacteria take over your mouth—like Porphyromonas gingivalis, a key player in gum disease—they can travel to your gut and disrupt its microbial balance. This dysbiosis (microbial imbalance) in the gut can lead to inflammation, increased intestinal permeability (leaky gut), and even contribute to chronic conditions like irritable bowel syndrome (IBS), Crohn’s disease, and metabolic disorders.
2. Immune System Interactions
Both the mouth and gut are key parts of your immune system. The bacteria that populate these areas can influence how your immune system responds to microbial assaults. Unhealthy oral bacteria can trigger systemic inflammation, potentially affecting how your body responds to infections and other inflammatory conditions in the gut.
Emerging research suggests that the oral microbiome might even affect the gut-brain axis—a communication network linking your brain and digestive system. Oral pathogens that enter the bloodstream or digestive tract can contribute to neuroinflammation, potentially influencing mood, cognition, and mental health.
3. The Role of Periodontal Disease
Periodontal (gum) disease is a prime example of how oral health can impact gut health. Studies have shown that individuals with chronic gum disease often have higher levels of harmful gut bacteria and systemic inflammation. Treating periodontal disease not only improves oral health but may also help rebalance the gut microbiome.
Supporting a Healthy Mouth-Gut Connection
Here are some practical steps you can take to foster a balanced oral and gut microbiome:
1. Maintain Good Oral Hygiene
Brush twice daily, floss regularly, and visit your dentist for routine checkups. This reduces harmful oral bacteria that could negatively impact your gut.
2. Assess Your Oral Flora with the DNA ConneXions Comprehensive Oral Test https://dnaconnexions.com/product/comp-oral-test/
If you’re curious about your specific oral bacteria, consider taking the DNA ConneXions Comprehensive Oral Test. This at-home test uses advanced DNA technology to identify a wide range (88 microbes total) of pathogenic microbes in your mouth. By understanding your unique oral microbiome, you can make more informed decisions about your dental care, diet, and overall health strategy.
3. Eat a Fiber-Rich, Low-Sugar Diet
Fiber feeds beneficial gut bacteria, while reducing sugar limits the growth of harmful microbes in both the mouth and gut.
4. Avoid Overuse of Antiseptic Mouthwashes
These can kill good oral bacteria along with the bad, potentially disrupting the microbial balance.
5. Consider Probiotics and Prebiotics
Oral and gut-targeted probiotics can support a healthier microbiome. Some supplements are specifically designed for oral health.
6. Reduce Stress and Get Enough Sleep
Chronic stress and poor sleep can alter microbial communities in both the mouth and gut.
Final Thoughts
The DNA ConneXions Comprehensive Oral Test screens for 88 pathogens, inclusive of anaerobic & aerobic bacteria, fungi, viruses, and parasites in removed teeth, oral blood, cavitations, tissue, dental implants, oral bone, saliva, and Super Floss samples. was designed to provide patients and practitioners a comprehensive view of patient health based on the oral flora. The report provided to the patient or practitioner provides information about each organism detected, the risk factors associated with that organism, and CDC recommended treatment protocols.
Your mouth and gut are more connected than you might think! A healthy oral flora supports a healthy gut microbiome, which in turn contributes to better digestion, stronger immunity, and even mental well-being. By taking care of your oral health, you’re not just protecting your smile—you’re nurturing your entire body from the inside out.