- 1 (888) 843-5832
- info@dnaconnexions.com

Acute Lyme disease refers to the early stage of infection that happens soon after a bite from an infected blacklegged tick. The bacteria most often involved is Borrelia burgdorferi. As the bacteria begin to spread, your immune system starts reacting.
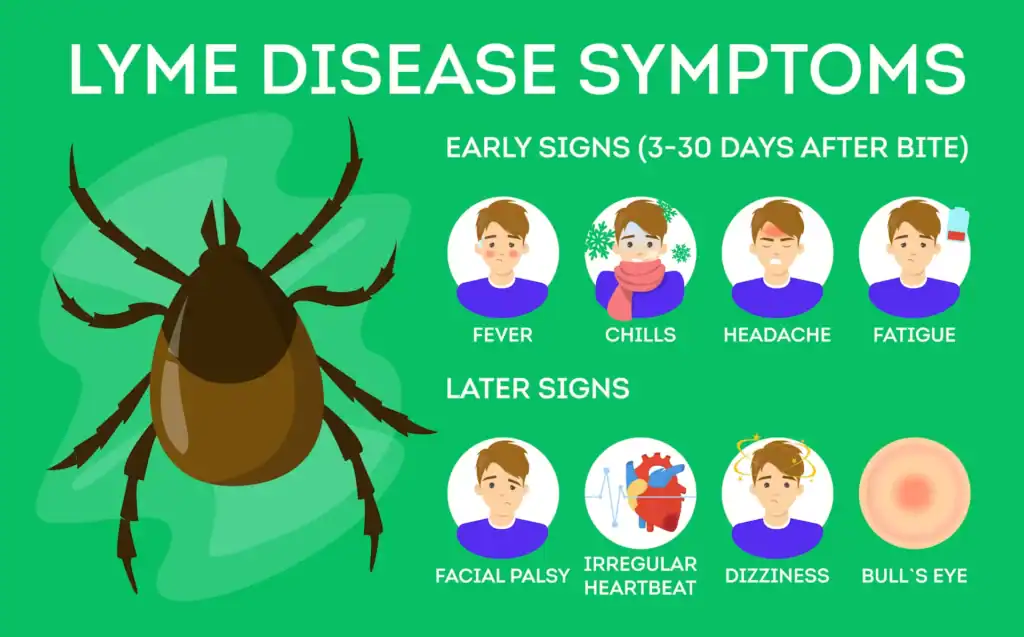
In the early weeks, symptoms can be easier to recognize. Many people feel flu-like symptoms. For example, fever, fatigue, headache, and muscle aches are common. Some people also notice swollen lymph nodes. However, these signs can look like a simple virus. So, it is easy to brush them off.
Then there is the rash that many people have heard about. It is called erythema migrans. The CDC says it occurs in over 70 percent of people with Lyme disease. Still, that means many people never see it.
Because early symptoms can look ordinary, acute Lyme sometimes goes unrecognized. When that happens, the timeline keeps moving.
Lyme disease is often described in stages. Still, it helps to think of it as a process that changes over time. At first, the infection may be more localized. Later, it can become more widespread.
Timing matters because the body’s signals change. Early on, you may have clearer signs like a rash or a sudden flu-like illness. Later, symptoms can become more scattered. They may also come and go. That shift is one reason people feel like they are chasing answers.
Timing also matters for testing. In the first few weeks, your immune system may not have made enough antibodies yet. The CDC notes that Lyme tests are usually serologic tests that detect antibodies, and antibodies can take several weeks to develop. Because of that, patients may test negative if they are recently infected.
If you test very early, a standard antibody blood test can miss the infection. That can be frustrating, especially if you feel awful and want answers.
This is one place where an at-home urine DNA-PCR test can be appealing. Instead of looking for antibodies, it looks for the DNA of Borrelia burgdorferi. It also checks for 10 common co-infections in the same panel.
In other words, it is a different kind of clue. Antibodies measure your immune response. DNA-PCR looks for genetic material tied to the organisms. So, when antibodies are not showing up yet, a DNA-PCR option can give another data point to consider.

When Lyme disease is not treated early, it does not always stay mild. Over time, inflammation can affect more than one system.
Some people develop joint problems. Others develop nerve symptoms. For example, numbness, tingling, facial weakness, or trouble thinking clearly can happen. When symptoms show up later, it can be hard to connect them back to a tick or mosquito bite from long ago.
That is why late symptoms often lead to the next big question: is this still Lyme, or is it something else?
Chronic Lyme disease is a term people often use when symptoms continue after an initial Lyme infection. It can also describe symptoms that return after treatment. Either way, the day-to-day impact can be real.
In medical settings, you may also hear the term Post-Treatment Lyme Disease Syndrome (PTLDS).
National Institute of Allergy and Infectious Diseases (NIAID) explains that most Lyme cases are treated successfully with antibiotics. Yet some patients continue to have symptoms like fatigue, pain, and joint and muscle aches after treatment. This is called PTLDS. NIAID
So, the label may change depending on who you talk to. Still, the experience is often the same. People feel unwell, and they want clarity.
Long-term symptoms often look different than early infection signs. Instead of a clear flu-like illness, symptoms may fluctuate. They may also overlap with other conditions.
Many people report:
Because these symptoms are not unique to Lyme, people can get misdiagnosed. They may also be told nothing is wrong. That can feel isolating.
At the same time, symptoms can have more than one cause. So, it is smart to keep a wide lens while you investigate.
Diagnosis gets more complex as time passes. One reason is simple. Most common Lyme blood tests look for antibodies, not the bacteria itself.
Antibodies can be helpful. A positive result can support that your body has seen Lyme before. However, antibody testing has a big limitation in long-term cases.
The CDC says it plainly: “Once elevated, antibody titers will remain so for months to years and cannot be used to determine cure.”
That is the confusing part for many people. If your antibody test is positive five years later, it can confirm past exposure. Still, it may not answer whether Lyme is active right now. In addition, if you were treated and improved, antibodies can still stay positive. So, the test can be “right” but still not settle the current question.
This is also why people sometimes feel stuck in a loop. They get a positive test and ongoing symptoms. Yet they still do not know what is driving those symptoms today.
In later-stage or long-term symptom cases, testing often becomes part of a bigger evaluation. A doctor may look at your symptom history, your exposure risk, and any objective signs on exam. Then testing can help support or weaken a Lyme explanation.
The CDC recommends a two-step testing process using FDA-cleared tests. People often call this two-tier testing.
When symptoms persist for months or years, people often want more than an antibody answer. They want a test that measures something different.
This is where an at-home urine DNA-PCR test can fit into the chronic symptom story. It does not rely on your immune memory. Instead, it is designed to detect the DNA of Borrelia burgdorferi. It also looks for 10 common co-infections in the same test. DNA ConneXions
That matters for two reasons.
First, if antibody tests stay positive for years, a DNA-PCR result can provide another angle. It can add a fresh piece of information to discuss with a provider. CDC+1
Second, co-infections can muddy the waters. Ticks can carry more than one pathogen. Symptoms can overlap and feel inconsistent. So, a panel that checks for Lyme plus common co-infections can help narrow the possibilities.
The difference between acute and chronic Lyme often comes down to timing and how symptoms evolve.
With acute Lyme, symptoms can be more recognizable. Treatment tends to be more straightforward when it starts early.
With longer-term symptoms, the story is rarely that simple. Symptoms may shift, overlap, or return. Testing can also be harder to interpret. Antibodies may not show up early, and they may stay positive for years later.
That is why people with long-term symptoms often want a testing approach that gives more than one signal.
Even with better testing options, early action is still a strong advantage. When people recognize symptoms early, they can seek medical care sooner. That can reduce the risk of late complications.
At the same time, it is important to be realistic. Early treatment improves outcomes for many people. Yet a subset of patients continue to have symptoms after treatment, as NIAID explains.
So, if you are dealing with lingering symptoms, you are not alone. And you are not imagining it. What you need is a clear plan to gather useful information.
Living with ongoing symptoms can feel like you are always explaining yourself. That is exhausting. Still, you can take steps that make the path clearer.
Start with what you know. Think about exposure risk and symptom timing. Then use testing to support smart decisions. Blood antibody tests can help show exposure, but they can stay positive for years.
When you want another type of data point, the DNA Connexions Lyme Disease Test can help you look for Borrelia burgdorferi DNA and 10 common co-infections in one panel. Most of all, it can help you have a more focused talk with your provider about what might be driving symptoms now. Chronic Lyme Disease vs. Acute Lyme is not always a simple story, but the right test information can make the next step feel less overwhelming.

In later-stage or long-term symptom cases, testing often becomes part of a bigger evaluation. A doctor may look at your symptom history, your exposure risk, and any objective signs on exam. Then testing can help support or weaken a Lyme explanation.
The CDC recommends a two-step testing process using FDA-cleared tests. People often call this two-tier testing.
When symptoms persist for months or years, people often want more than an antibody answer. They want a test that measures something different.
This is where an at-home urine DNA-PCR test can fit into the chronic symptom story. It does not rely on your immune memory. Instead, it is designed to detect the DNA of Borrelia burgdorferi. It also looks for 10 common co-infections in the same test. DNA ConneXions
That matters for two reasons.
First, if antibody tests stay positive for years, a DNA-PCR result can provide another angle. It can add a fresh piece of information to discuss with a provider. CDC+1
Second, co-infections can muddy the waters. Ticks can carry more than one pathogen. Symptoms can overlap and feel inconsistent. So, a panel that checks for Lyme plus common co-infections can help narrow the possibilities.
The difference between acute and chronic Lyme often comes down to timing and how symptoms evolve.
With acute Lyme, symptoms can be more recognizable. Treatment tends to be more straightforward when it starts early.
With longer-term symptoms, the story is rarely that simple. Symptoms may shift, overlap, or return. Testing can also be harder to interpret. Antibodies may not show up early, and they may stay positive for years later.
That is why people with long-term symptoms often want a testing approach that gives more than one signal.
Even with better testing options, early action is still a strong advantage. When people recognize symptoms early, they can seek medical care sooner. That can reduce the risk of late complications.
At the same time, it is important to be realistic. Early treatment improves outcomes for many people. Yet a subset of patients continue to have symptoms after treatment, as NIAID explains.
So, if you are dealing with lingering symptoms, you are not alone. And you are not imagining it. What you need is a clear plan to gather useful information.
Living with ongoing symptoms can feel like you are always explaining yourself. That is exhausting. Still, you can take steps that make the path clearer.
Start with what you know. Think about exposure risk and symptom timing. Then use testing to support smart decisions. Blood antibody tests can help show exposure, but they can stay positive for years.
When you want another type of data point, the DNA Connexions Lyme Disease Test can help you look for Borrelia burgdorferi DNA and 10 common co-infections in one panel. Most of all, it can help you have a more focused talk with your provider about what might be driving symptoms now. Chronic Lyme Disease vs. Acute Lyme is not always a simple story, but the right test information can make the next step feel less overwhelming.